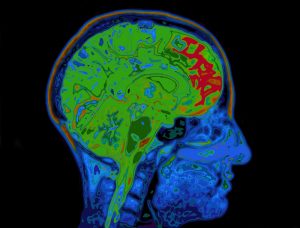
New research shows that neurons in the preoptic hypothalamus – the region of the brain that regulates sleep and body temperature – are rhythmically activated during non-rapid eye movement (NREM) sleep. According to a study published in Current Biology from the Perelman School of Medicine at the University of Pennsylvania, stress activates these brain cells uncontrollably, causing “micro-arousals” that disrupt sleep cycles and shorten the duration of sleep episodes.
What Happens in the Brain During Sleep
While our body rests during sleep, our brain is still very active in four different stages of sleep. In each 90-minute sleep cycle, there are three stages of NREM sleep and one stage of REM (Rapid Eye Movement) sleep. While REM sleep is characterized by rapid eye movements, in the non-REM phase there is a decreasing activity in the brain, in which the muscles relax more and more until deep sleep finally occurs. Previous research has shown that a broad network of neurotensin-producing neurons is involved in NREM sleep regulation. These neurons usually express the gene that encodes the neuropeptide neurotensin. Activation of these neurons triggers non-REM sleep.
Understanding the biology that drives brain activity during these crucial sleep phases and how stimuli such as stress can disrupt them is critical so that therapies can one day be developed to help people get the more restful sleep that their brains need allows these important processes to be completed.
Developing Treatments for Stress-Related Sleep Disorders
The University of Pennsylvania researchers monitored activity in the preoptic area (POA) of the hypothalamus of mice during their natural sleep and found that glutamatergic neurons (VGLUT2) are rhythmically activated during NREM sleep. They also found that VGLUT2 neurons were most active during wakefulness and less active during NREM and REM sleep. During microarousals in NREM sleep, VGLUT2 neurons were the only active neurons within the POA, and their signals began to increase in the period before microarousal. To confirm that active VGLUT2 neurons were indeed the cause of microarousal, the researchers stimulated VGLUT2 neurons in sleeping subjects, which immediately resulted in an increase in microarousal and wakefulness.
To illustrate the connection between stress and increased VGLUT2 neuron activation, the researchers then exposed subjects to a stressor that increased wake time and microarousals, and decreased total time in REM and NREM sleep. The researchers also found increased VGLUT2 neuron activity during NREM sleep in the stressed volunteers. Additionally, when the researchers inhibited VGLUT-2 neurons, microarousals during NREM sleep decreased, and NREM sleep episodes were longer. The glutamatergic neurons in the hypothalamus offer a promising target for developing treatments for stress-related sleep disorders, according to the researchers. The ability to reduce interruptions during key periods of non-REM sleep by suppressing VGLUT2 activity would be groundbreaking for people struggling with sleep disruption due to disorders such as insomnia or PTSD.







