Scientists at Duke-NUS Medical School have identified a gene that controls the behavior of a specific type of cardiac macrophage, which is responsible for excessive scarring in the early stages of common heart disease, or cardiomyopathies (various heart muscle diseases). When the gene called WWP2 (an E3 ubiquitin protein ligase) is blocked, heart function improves and scar tissue formation slows down, slowing the progression of heart failure.
Function of WWP2 in fibrotic diseases
Scarring or fibrosis of the heart, as in non-ischemic cardiomyopathies, is a progressive condition and a global health problem,” said Associate Professor Enrico Petretto, Director of the Duke-NUS Center for Computational Biology and a systems geneticist at the School’s Cardiovascular & Metabolic Diseases (CVMD) program.”In its earliest stages, it is characterized by an inflammatory phase, so intervention at this point could significantly delay the progression of the disease”
Petretto and colleagues in Singapore, China and the UK have studied the function of WWP2 in fibrotic diseases for several years and first discovered that it is a key driver of scar formation when expressed in fibroblasts – the cells that form scar tissue. In their latest findings, published in Nature Communications, the team turned to the early stages of the disease.
WWP2-expressing macrophages promote scar formation
Using single-cell RNA sequencing, the team found that when fibrosis is triggered, a variety of different macrophages, immune cells that clear foreign bodies in the body, are activated in a preclinical model of heart disease. While macrophages are best known for their role in clearing away cancer cells, microbes, and cellular debris, they also help regenerate healthy muscle cells.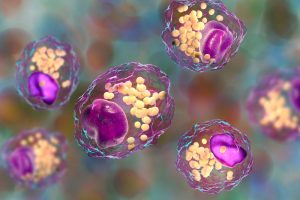
However, a subset of these cardiac macrophages are controlled by WWP2. These WWP2-expressing macrophages actively promote scar formation by inducing local heart cells (fibroblasts) to produce collagen out of control, which promotes scar tissue formation. Researchers found that: “When WWP2 is expressed in macrophages, these cells ‘irritate’ fibroblasts, leading to uncontrolled scarring.”
Small molecule inhibitor blocks WWP2
In contrast, when macrophages did not express WWP2, the team observed reduced infiltration of pro-fibrotic macrophages into the heart and the effect of repair macrophages was better maintained, with clear beneficial effects on heart tissue and heart function in the later stages of the disease.
“Targeting WWP2 is like throwing a blanket over the fire — it deprives the flames of oxygen before the whole house burns down,” CVMD program systems biologist Associate Professor Jacques Behmoaras, a co-corresponding author of the study, explained. Blocking the function of WWP2 in this subset of cardiac macrophages is sufficient to slow or even stop scarring.”
The team is developing a small molecule inhibitor against WWP2 that can do just that. Rather than indiscriminately depleting all macrophages, which has shown deleterious effects, the Duke-NUS team targets WWP2, which acts specifically on these pro-fibrotic macrophages and activated fibroblasts to halt scarring of the damaged heart.
Promising therapeutic potential
“Because WWP2 plays a dual role in scar tissue formation, blocking it by dampening inflammation and scarring all at once kills two birds with one stone. And with its added benefit of promoting beneficial tissue repair macrophages, WWP2 becomes a very attractive therapeutic target.
Researchers are now in the process of creating small molecule inhibitors targeting a specific form of the WWP2 protein, which have already shown promising antifibrotic results in cells. They posit that this could have therapeutic potential for treating fibrotic diseases such as non-ischemic cardiomyopathies, and could prove effective in other fibrotic diseases involving WWP2.






